One baby, three parens: Doctors made this possible using an innovative IVF technique preventing mothers from passing genetic diseases on to their babies.
- In 2019 a healthy baby with DNA from three parents was delivered in Greece.
- The procedure that made this possible is called ‘Maternal spindle transfer’. It was initially developed to help mothers with mitochondrial genetic disorders to have healthy children.
- Experts are concerned about the use of mitochondrial donation for infertility issues.
Last year, a healthy baby boy, weighing 2.9kg (6lbs), with DNA from three parents, was born in Greece, TIME reveals. As researchers at the Institute of Life in Athens announced, the mother of the wonder-child was a 32-year-old Greek woman with a history of several unsuccessful cycles of in vitro fertilization(IVF).
The child was born on April 9, 2019, with an experimental technique called ‘maternal spindle transfer’.
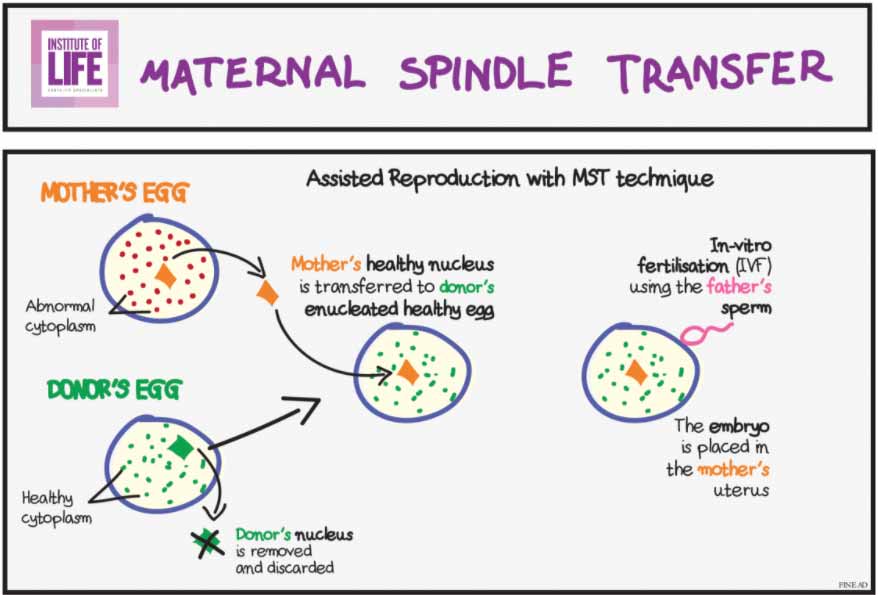
The procedure includes removing the grouped-together DNA from a mother’s egg and placing it inside a donor egg from another woman. This donor egg was previously emptied of its DNA. After that, it was fertilized and developed into an embryo that was transferred for pregnancy. Although the child technically has three parents, he will mostly have DNA from the biological mom and dad.
The whole process aims to help mothers with mitochondrial genetic disorders to have healthy babies.
Mitochondrial DNA is responsible for less than 1% of a person’s total genetic makeup, but inherited mutations in this DNA can cause severe and sometimes life-threatening mitochondrial diseases.
According to Dr. Panagiotis Psathas, president of the Institute, it is also applicable to women who have struggled to conceive. Dr. Psathas explained:
“We are now in a position to make it possible for women with multiple IVF failures or rare mitochondrial genetic diseases to have a healthy child. At the Institute of Life, our commitment is to continue to help even more couples facing fertility issues to have children with their own DNA, without having recourse to egg donors.”
As per One Zero, at least ten babies with three parents were born by September 2019. While this sounds revolutionary, experts are warning the procedure might be dangerous.
The European Society of Human Reproduction and Embryology (ESHRE) recommends ‘extreme caution’ on the use of the technique after failed IVF cases. They said in a statement:
“ESHRE strongly discourages the use of mitochondrial donation to alleviate an infertility condition.”
However, the case reported in Greece was of a mother who did not have any mitochondrial disorders. She was unable to conceive after four IVF cycles and decided to take part in the experimental study. The Greek institute was working in collaboration with the Spanish company Embryotools, which developed the technology.
Dr. Nuno Costa-Borges, a co-founder of the Spanish company, noted:
“The completely successful and safe implementation of the Maternal Spindle Transfer method – for the first time in medical history – is a revolution in assisted reproduction.”
Nine more babies have been born after their mothers underwent the procedure for infertility.
Despite the controversial statements of various experts, as of September 2019, there was a total of ten children delivered to mothers with infertility troubles. Apparently, and that more three-parent babies are likely on the way. The nine other cases occurred at Nadiya Clinic in Kyiv, Ukraine, according to Dr. Valery Zukin, the center’s director.
Having in mind that that faulty or fewer mitochondria could be a cause of poor-quality eggs, some experts claim that the experimental technique may boost the chances of a successful pregnancy after failed IVF.
On the contrary, reproductive specialists say there’s not enough evidence to know whether mitochondria are responsible for all cases of age-related fertility. Moreover, other professionals claim mitochondrial replacement therapy to be a form of genetic modification.
Another concern experts have about the procedure came as a study published in Science suggests that mitochondria are not readily interchangeable and thus could not be replaced with those from a donor with no consequences.
The study reveals that the donor might need to have a similar genetic makeup to the woman undergoing the procedure.
Examining more than 1,500 mother and child pairs, the researchers found subtle connections between their mitochondrial DNA and their nuclear DNA. Patrick Chinnery, one of the authors of the paper, said:
“Swapping mitochondria might not be as straightforward as just changing the batteries in a device.”
As there are several different perspectives on the subject, there are different reactions to the innovative method as well.
For instance, in 2015, the US has banned the mitochondrial replacement therapy wit a bill passed by Congress. On the other hand, the same year, the UK made the therapy legal, but only for couples at high risk of having a child with a life-threatening mitochondrial disease.
Costa-Borges of Embryotools said:
“In general, we agree that this is still an experimental technique and thus we need to keep on with our research to provide all evidence about the effectiveness and safety of the procedure for infertility problems. Only groups with demonstrated experience should be conducting this type of research, as regular IVF centers usually do not have the equipment and expertise needed.”